A Guide to PSA Testing for Primary Care Providers
PCPs play crucial role in reducing late-stage prostate cancer diagnoses.
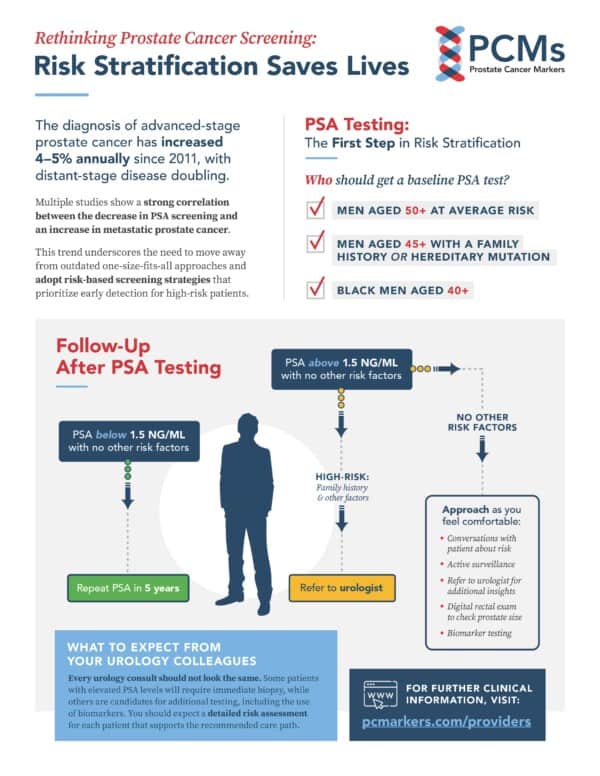
Despite recent declines in overall cancer mortality rates, advanced-stage prostate cancer diagnoses are on the rise. Multiple studies have shown a strong correlation between the decrease in PSA screening in recent years and an increase in metastatic prostate cancer diagnoses.
Primary care providers (PCPs) order 90% of PSA tests, making them the front line of early cancer detection. It’s essential for PCPs to recognize the vital role of PSA testing in early prostate cancer detection.
Adding PSA Back to Your Assessment Tool Kit
At annual preventive exams, PCPs order tests to assess the risk of common diseases and determine if follow-up diagnostic testing or intervention is necessary. PSA testing works the same way: It doesn’t diagnose prostate cancer but helps identify patients who may require further evaluation.
Think of it like testing blood sugar levels. Elevated PSA levels warrant further investigation, just like high blood sugar triggers follow-up A1C testing.
With the development of additional diagnostic tests, including MRI and biomarker testing, plus a better understanding of risk stratification, PCPs can help identify early stage prostate cancer without the fear of overdiagnosis and overtreatment as in the past.
“It’s heartbreaking to hear patients ask how long cancer has been present when it could have been caught earlier with a simple test,” says Michael Liss, MD, PhD, MAS, FACS, a urologic oncologist at UC San Diego Health and a member of the PCMarkers Scientific Advisory Board.
Setting a Baseline PSA; Identifying High-Risk Patients
Our mission at PCMarkers is to save men’s lives by detecting and effectively treating clinically significant prostate cancer early. As part of this mission, we are committed to reducing unnecessary test and treatment, including prostate biopsies, by guiding PCPs and urologists in the effective use of biomarkers, including the PSA test.
Download the PSA Testing Algorithm
Baseline PSA testing is essential to establish in all adult male patients. This test can help you categorize your patients into risk pools to focus your limited time on patients who need a closer look.
We recommend ordering baseline PSA tests for:
- Men age 50+ at average risk
- Men age 45+ with a family history or hereditary mutation
- Black men age 40+
An average of 3 out of 4 men will have a PSA below 1.5 ng/ml. With no other risk factors, we recommend putting these patients in your low-risk pool and repeating PSA testing in five years. (We recommend 1.5 ng/ml vs. the standard 4.0 ng/ml due to an expansive study performed by Dr. E. David Crawford showing that this lower cutoff still appropriately filters low-risk candidates while capturing an important group of patients who would be missed with the higher cutoff. However, we recognize as urologists that we have overwhelmed PCPs with conflicting advice and urge all PCPs to choose a cutoff between 1.5 and 4.0 ng/ml that they are comfortable with using consistently.) Family practice doctors and patients need a simple and accurate cutoff and while not perfect, 1.5 ng/ml is the level, states Dr. Crawford.
Most Elevated PSAs Don’t Warrant Immediate Urology Referrals
In most cases, PCPs should consider additional follow-up steps to an elevated PSA result before making a urology referral. If a patient has known risk factors (family history of cancer, genetic mutation, African descent, age over 65) and a PSA above 1.5 ng/ml, you may want to consider a urology referral but request a risk assessment outlining the recommended follow-up testing.
“Urologists need to earn the trust of our primary care providers by ensuring that a referral for an elevated PSA or assistance with screening does not mean immediate prostate biopsy and needless testing,” Dr. Liss says.
For patients with PSA levels above your comfortable cutoff (again, we recommend 1.5 ng/ml), you may want to consider these follow-up steps:
- Digital rectal exam (DRE) to assess prostate size (86% of men with BHP have elevated PSA levels)
- Assessment of family history, with consideration of genetic testing
- Active surveillance, with repeat testing in 3-12 months
New Alternatives to Biopsy for Elevated PSA
PSA testing has faced legitimate criticism due to past practices, where elevated PSA levels and abnormal DREs often led to prostate biopsies resulting in overdiagnosis and subsequent treatment of nonmalignant prostate cancer.
Today, both PCPs and urologists share responsibility to appropriately screen for risk and use all available tools to determine whether a man should receive further testing or biopsy and treatment. We cannot emphasize enough that the PSA test is a legitimate and important screening tool that can and should be used as a low-cost, simple method to help detect the potential of prostate cancer.
From this starting point, PCPs and urologists then can collaborate to leverage advances in prostate cancer testing to better inform clinical decision making.
Rethinking Prostate Cancer Screening: Risk-Stratified PSA Testing for PCPs